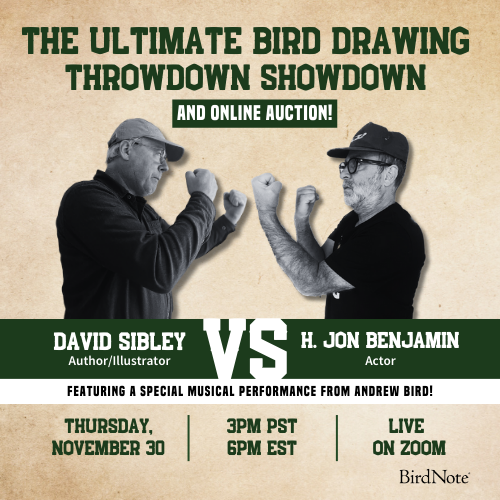
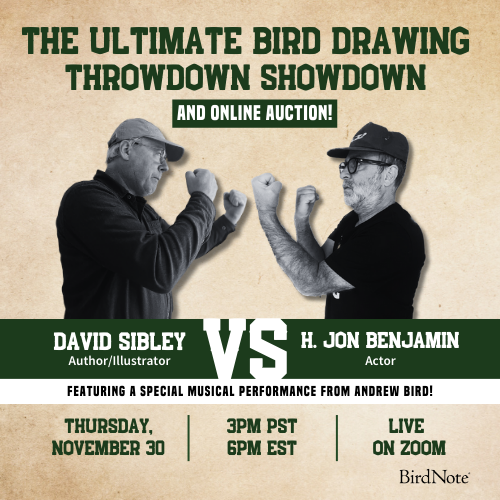
Join BirdNote tomorrow, November 30th!
Illustrator David Sibley and actor H. Jon Benjamin will face off in the bird illustration battle of the century during BirdNote's Year-end Celebration and Auction!

Avian flu, better known as bird flu, has been in news headlines all of 2024. Still, many questions remain for the general public. What is it? What’s causing it? How is it spreading? And how serious should we be taking this public health matter? Our co-hosts Purbita Saha and Deja Perkins sit with leading scientists, Director of Molecular Biology Dr. Andy Ramey from the USGS Alaska Science Center, and molecular virologist at Tufts University, Dr. Wendy Puryear. Tune in. Share with a friend. And don’t fret, our only goal is to leave you like an owl– very sharp, very wise.
Want more Bring Birds Back? Subscribe to our show and follow us on Instagram! For more about BirdNote, sign up for our weekly newsletter. And for ad-free listening and other perks, sign up for BirdNote+ here.
BirdNote is a nonprofit. Your tax-deductible gift makes these shows possible.
Bring Birds Back Special Season 6 is sponsored by the Cornell Lab of Ornithology and the American Bird Conservancy.
Purbita Saha: BirdNote Presents.
[Bring Birds Back Stinger]
Purbita Saha: From BirdNote, this is Bring Birds Back. I’m Purbita Saha.
[Music starts]
If it's not one thing, it's another. The seasonal flu, the common cold, RSV, COVID, West Nile — with so many viral threats constantly in rotation, it can be hard to keep track. You may have heard of “bird flu” in the news or wondered why eggs and poultry prices have skyrocketed in recent years.
Well, we’re now more than two-and-a-half years into an outbreak. Since January 2022, the virus that causes bird flu has infected millions of wild and domestic birds around the world and dozens of mammal species, including humans. But two-and-a-half years doesn’t feel so long compared to the 150-year-long quest to learn how this virus spreads and kills — and whether it can be stopped for good.
Bird flu was first identified by an Italian parasitologist in the 1870s. At the time, the contagion was dubbed the “fowl plague” because of its deadliness among chickens and other poultry. In 1955, scientists realized the sickness was caused by a type of influenza virus — not a bacteria, as previously thought. And in 1981, they officially named it Highly Pathogenic Avian Influenza, or HPAI. (In this episode you’ll also hear it referred to as HiPath, avian flu, and H5N1.)
By now, the world has battled many strains of bird flu, though none as infectious and vicious as the one we’re dealing with today. But with each new case, scientists are getting closer to finding out how the virus evolves.
For this episode, my co-host Deja Perkins and I spoke with two experts on the frontlines of the current bird flu outbreak to really understand the virus.
First, let's get to know a bit more about each guest:
I had the pleasure of speaking with Dr. Andy Ramey, a research wildlife geneticist with the Alaska Science Center for the United States Geological Survey or the USGS. He currently serves as the director of the center’s Molecular Ecology Lab.
Andy Ramey: We interact with animals in a lot of different ways, sometimes we actually capture animals to understand, for instance, if they are infected with avian influenza viruses and that requires taking some swab samples. Sometimes we might take a blood sample to assess if they have antibodies that indicate prior exposure to avian influenza.
Other times our studies might be more observational, sometimes we sample wildlife habitats, it really depends on the research question.
Purbita Saha: My co-host, Deja Perkins, spoke to Dr. Wendy Puryear, a molecular virologist at the Tufts University School of Veterinary Medicine. Though Wendy and Andy do similar things, they have different areas of expertise.
Andy's work studies the effects of viruses in hosts over a period of time, while Wendy's work focuses on the virus itself — specifically influenza in birds and mammals.
Wendy Puryear: It can be live birds, it can be dead birds, it can be sick birds, and it can be also going out to locations and literally collecting fecal samples and testing those too. Now that we have all collectively lived through the COVID pandemic we are all familiar with what it means to be tested for a virus by PCR.
And really, that's the same thing that we do with the birds. It's the same swab. So, those swabs are used to swab birds that are either coming into a rehab facility for any number of reasons: because they were found sick or maybe they were entangled in a fence, or it was a car strike.
So it isn't necessarily that they are birds that are found dead, it can be coming in for any reason. So it might be bird banding or monitoring a population for any number of reasons.
So all of those are populations of birds where we can collect swabs. And from that swab, you can then go and extract out the viral RNA, to actually look and see, can we specifically detect influenza? And once we detect it, we go in and more specifically ask, is it that bird flu form of influenza?
Purbita Saha: So, you heard the origin story of bird flu earlier — but that history is from well over a century ago. The current strain, H5N1, only goes back a couple decades.
Wendy Puryear: Oh, let's see. Bird flu or HiPath influenza or H5N1— they're all talking about the same outbreak that we currently have going on, really around the globe.
And this form of the outbreak, it really started going all the way back to 1996 that this virus first emerged, uh, into birds. So, it started out in farmed poultry.
And this was in China, it took about 10 years or so before it then went into wild birds and even then it stayed fairly local. It took another 10 years or so before I got into migratory birds and started to spread around the globe. And it has been circulating in Europe and in the Arctic for, you know, the last 20 years or so.
But it was in 2014, 2015 that a precursor - it's not the exact same one - but sort of an ancestor of it, came into North America. We did have an outbreak, but we controlled it pretty quickly, and we never saw it again.
It did continue to circulate, though, in Europe and in the Arctic, but we didn't see it in North America again after that. And then in late 2021/early 2022, it shifted and it came back in again, Transatlantic. It came across the Atlantic Ocean, came into kind of Atlantic Canada and just took off.
So it was a matter of two to three months before it first landed here and had spread all the way across North America. In that spread, came with a large amount of mortality in both wild birds and in domestic birds. And it very quickly started spreading into mammalian species as well.
So a lot of those were individual spillover events, but it was happening fairly frequently. And that's not something that influenza has done on a regular basis before.
[Music start]
Purbita Saha: A spillover event occurs when one animal species, such as a bird or a cow, unexpectedly transmitsa virus to a new type of host, like a human. And the opposite of that event is called a spillback, like when a virus moves from a human back to its original animal host- sometimes without even causing any symptoms.
Those early spillover events for bird flu have multiplied in recent years. So, what's different now?
Andy Ramey: So we've known for a very long time, for many decades that influenza A viruses are common among wild birds, specifically among wild waterfowl.
Purbita Saha: Influenza A viruses are the reason humans get illnesses like the common flu, pneumonia and ear or sinus infections. These viruses often start out circulating through animal hosts, like waterfowl and pigs, that later pass them on to humans.
Andy Ramey: Those viruses typically do not cause disease, they are low pathogenic meaning that they cause little to no disease in chickens. And are, therefore, not very economically costly.
However, some small set of these low pathogenic viruses, can evolve to cause serious disease and death among affected chickens. So that's really where the chicken became the, sort of, litmus of pathogenicity because outbreaks of highly pathogenic avian influenza, meaning that they cause severe disease and death among chickens, are extremely costly to industry.
So this lineage of virus emerged in Guangdong, China and caused, actually, a cluster of human disease in that region. And has since spilled over numerous times into wild birds. And that's pretty novel.
Uh, it's been historically very uncommon for highly pathogenic avian influenza to spill from domestic birds, back into wild birds. But this particular lineage has spilled back numerous times. And through the course of these numerous spillbacks, has now become established among wild birds.
And that's become a big deal in a way that has no precedent. So, it's become much more common and therefore causing much more disease among domestic animals as well as wild animals.
Purbita Saha: While there’s no clear explanation as to why these changes are occurring, Wendy says bird flu experts do have a few ideas.
Wendy Puryear: Why exactly that change is something that is an open question and a lot of people, our group included, are trying to figure out. Why is it able to go into so many mammalian species? Why are we seeing it in dairy cattle now? So it's just, kind of, thrown out all of the rule books. But part of it may also be: it is in a lot of different species and that is a feed forward loop in the ecosystem. If you have a bunch of sanderlings that are infected with high path influenza and they're being preyed upon by owls or whatever it is, that feeds up into those species and then that feeds forward and that feeds forward
Part of it is that it's potentially being amplified through the ecosystem as we've had this large amount of die off.
[Music stops]
Purbita Saha: So, how contagious is bird flu and how does it spread among birds? Wendy says it usually infects their gastrointestinal tracts.
Wendy Puryear: So it's something that is spread through fecal. It's shed into the water and then they're dabbling down in there and you end up getting the propagation of the virus through the ecosystem through that way. And if you picture a relatively small pond and you have an infected duck that comes in and they're shedding a large amount of virus and there's a bunch of other ducks that are in there, a lot of those animals are going to end up becoming infected.
But if you have something where they're more spread out and you're not having a lot of direct interaction. So if you have a bald eagle that's infected, they may bring it back to their nest. And we see that sort of scenario where chicks will then become infected and you might lose a whole nest and the parents, but they're not necessarily spreading on to a bunch of other eagles.
So it, it differs a little bit depending on the species. But with that said, it can be incredibly infectious. There's a lot of examples where influenza will land on a colony, and then in a matter of a week or two, most of that colony can be wiped out by influenza. So there's, you know, one example of, of turns on an island off of Washington state where it was, 1,700 terns just died over the course of a week, all from influenza just landing on that colony. Or when it got into pelicans in South America and you have tens of thousands of birds that die over the course of a couple of weeks.
So it can really go through like wildfire when it lands in those colonially nesting species that are in close proximity to each other.
Purbita Saha: Are there any particular birds that are more at risk for getting bird flu?
Andy Ramey: Waterfowl are traditional, reservoir hosts for Influenza A viruses and we've seen a fairly large number of waterfowl affected by Highly Pathogenic Avian Influenza, but often these birds appear perfectly healthy when they are infected.
And we know this through sampling of live captured birds as part of, say, banding operations and also, hunter harvested birds, say from duck hunting. Much of what we know about other species being infected by highly pathogenic avian influenza is through what's called passive surveillance. That is when people come across sick and dead birds.
So, species that have been identified as affected through passive surveillance have included raptors, there's been a fairly large number of raptors, such as bald eagles, that have been found sick and that have died. And also seabirds is another general type of bird that there's been fairly large numbers of detections. That being stated, I think there's a great diversity of birds that have been affected.
I've heard globally it's approximately 500 different taxa, so I think any sick or dead bird could and perhaps should be considered suspect for infection with highly pathogenic avian influenza. I haven't seen large numbers of songbirds reported as confirmed.Historically, there's evidence that not many songbirds are exposed to influenza viruses and that could be that these viruses are typically spread through water and many songbirds aren't interacting heavily with water sources, like large wetlands, that is.
However, there also could be a detection bias. Songbirds are pretty small and they would be pretty hard to encounter or to find if they're sick or have died. So there could be a reporting bias in songbirds that have been affected by highly pathogenic avian influenza and people should be aware of that.
Purbita Saha: Andy strongly encourages folks to take the current numbers with a grain of salt:
Andy Ramey: They're probably good estimates, but underestimates of the actual disease burden on the landscape.
[Music starts]
Purbita Saha: A disease burden is a calculated measure of how a health concern, such as a potentially deadly virus, can harm a population. In this case, it refers to infection and mortality rates in wild birds, poultry, and all the other species impacted by bird flu.
According to the CDC and US Department of Agriculture, as of October 2024, 103 million birds have been detected with H5N1 in the past two and a half years. These stats come from 48 states, 530 counties and more than eleven hundred reported outbreaks.
One report from the USDA describes the current avian flu outbreak as the largest and longest outbreak that our country has ever seen, which is a bit concerning. What's happening there?
Andy Ramey: From a wildlife perspective, highly pathogenic avian influenza is now affecting more wild mammals than we've ever seen in the past. Here in the United States, there's been much more than prior accounts.
Wendy Puryear: The last time I had looked, and this is changing on a regular basis, I think there are at least 60 different species of mammals that have been infected by high path influenza.
There've been some goats, there've been some llamas; marine mammals have been one of the mammalian species that have probably been the hardest hit so far by high path influenza. The largest die offs were in South America, but where there's tens of thousands of marine mammals that will die over the course of a short period of time from high path influenza, going into those species. So it's been in seals and dolphins, several different species of bear, in cats and dogs and squirrels, opossums, raccoons, skunks, bobcats, and the list goes on and on. The most unusual one that is currently making a splash on the radar is dairy cattle.
It is making its way through the food chain and into a lot of unexpected places. The, the cattle one was a definite curveball. That was not one that really anybody saw coming.
Purbita Saha: So, how does this happen? While avian flu spreads from bird to bird through feces, Wendy says it works differently in mammals.
Wendy Puryear: So generally speaking, in mammals, including us, it's respiratory.
So either, it's inhaled, or through eyes, or whatever mucosal surface is a way that it can get into us and other mammals. It's not as completely straightforward as that. You can get both forms of transmission happening in both categories of species. But another thing that you're starting to see more of with this high path virus is through direct ingestion. So if a fox eats an infected bird, then they're getting infected. They could be getting it into their mucosal surfaces. Either while they're consuming a prey or if they're going through an area that is contaminated because it has been shed in the feces of the bird.
Between birds and marine mammals, virus that’s shed either in shallow water or on the rocks or on the beach, a seal will come through it and aerosolize and inhale that as they're going through the fecal matter. So, both ways are possible ways that you can end up getting from a bird to a mammal.
[Music stops]
Purbita Saha: Particularly for humans, as Wendy mentioned, bird flu spreads similarly to COVID– which infects your respiratory system. The virus can get in through your eyes or through any place that secretes mucus, such as your mouth, nose, lungs, and stomach. As for birds and animals, there are some pretty recognizable symptoms.
Wendy Puryear: So it's not absolute, but in a lot of cases, there's that really strong neurologic involvement. So, in the majority of both avian and mammalian cases, for example, with birds either unable to fly, they might be kind of moving around in circles on the ground or in the water, unable to hold their head up, kind of flopping their head around, similar sorts of things, seizures that show up in mammals, and that same sort of kind of atypical neurologic sort of movement.
And then sometimes there's a— an involvement in the eyes. Um, that's been seen in some birds where actually the eye color changes and a lot of cases it's fatal. So it's generally pretty apparent when an animal is infected.
What I've come to learn over the course of this outbreak is there's actually a lot of things that cause neurologic symptoms in birds. So, just because the bird is neurologic doesn't necessarily mean it's high path. It could be a number of other things that are causing that, but high path generally is neurologic.
Ducks, generally speaking, tend to not be as clinically affected. Cows, however, have not had any of these symptoms. So it had seemed like it was pretty consistent that you would see these neurologic signs when an animal was infected with high path. Cows show none of that. So it's possible that there are other species that we just don't realize are being impacted by the virus and they're not presenting in the same way and they haven't been kind of tested and come across yet.
Likewise with birds, it's possible that there are some asymptomatic hosts that are out there. Most of them, it's visually obvious that they're infected.
Purbita Saha: Andy, do you have any other major concerns about bird flu and how fast it’s spreading?
Andy Ramey: Of course something that we're all keeping our eyes on is the potential for highly pathogenic avian influenza to become a pandemic influenza strain among humans. So, there is not any evidence that has occurred yet, but small numbers of humans are being infected and it's something that the world and various world health organizations are keeping a close eye on and making preparations for.
Purbita Saha: After the break, my co-host Deja asks the hard-hitting questions about virology, vaccines and more; and later, I'll be back to share more about safety and why you should be aware, but not worried.
After these messages…
MIDROLL
Deja Perkins: And we’re back. I’m Deja Perkins and we’re speaking with Andy Ramey, a research wildlife geneticist, and Wendy Puryear, a molecular virologist.
Now, let’s dive a bit deeper into the bird flu— on its threat level, the potential use of vaccines, prevention tips and more. Starting with the worry that many of us have: another potential pandemic.
Andy Ramey: In the United States, all the human cases of which I am aware have had to do with interactions of humans with infected domestic animals. That is, there's been a small number of cases of humans interacting with infected domestic poultry and a small number of cases of humans affected, based on their interactions with infected domestic dairy cattle. In all cases, to my knowledge, a disease has been relatively mild conjunctivitis or pinkeye and mild respiratory disease. To my knowledge, all human cases have resolved on their own or with minimal health intervention and everyone survived and is healthy today.
[Music start]
Deja Perkins: To be clear, Andy is only talking about cases in the United States. As of October, 2024, 36 cases of bird flu reported in this country were human affected. Almost all cases were confirmed spillovers from farm-related H5N1 outbreaks this year and every person recovered.
However, the mortality rate hasn’t been as hopeful on a global scale. Between January 2003 and July 2024 — a span of over 21 years — there have been 896 reported cases of bird flu infection in humans, with 463 reported deaths — giving the virus a 52% fatality rate for humans globally.
Wendy Puryear: If you go back all the way to the mid nineties, when it first emerged, and look at the whole swath— it's been 50 percent or so mortality in humans, but it's been a small number of people that have been infected.
So it's not something to be super panicked about but it's also not something to put our head in the sand and not pay any attention to and not put any resources into. We want to be able to pay really close attention to whatever changes are happening with the virus that might shift it to a place where it's no longer a total of a hundred and now we start to see higher numbers.
It's that line between don't panic, but don't ignore it.
Deja Perkins: And Andy says that the current strain of bird flu is far-reaching.
Andy Ramey: This is really a global problem right now. In fact, every region of the world has been affected by this panzootic, the animal equivalent of a pandemic, of highly pathogenic avian influenza with the exception of Australia and some areas of Oceania. So animals on most continents and in most regions have been affected in one way or another.
Wendy Puryear: It's actually been inspiring and encouraging to see just how much collaboration there is really across the globe, Literally, regular weekly meetings of representatives from all over the place sharing information about where active outbreaks are and trying to work collaboratively as quickly as possible. So there's a lot of really coordinated efforts to try as best as we can to pool all those resources and expertise, stay on top of it and figure out how best to respond.
Deja Perkins: While it’s comforting to hear that this issue is being tackled worldwide, due to the ongoing concerns regarding bird populations, the threat to conservation is very much a reality.
Andy Ramey: We know that large numbers of birds have died and that birds are continuing to have died. So, absolutely there's a conservation concern. I think, fortunately, the numbers of birds and the species of birds that have died have tended not to be those populations that are of highest conservation concern. I have yet to see any reports of large numbers of threatened or endangered species that have been affected with maybe the single exception of California Condors.
Deja Perkins: The California Condor is among the first birds to ever receive federal protection in the United States and has been considered critically endangered or at high-risk of extinction since 1967.
Following studies in the early 1970s, when biologists determined less than 30 California Condors remained, a major conservation effort went into effect in an attempt to save the species.
Now, more than 500 California Condors exist and over half of them are in the wild. Still, they have quite a long way to go and remain federally protected and closely monitored.
[Music stops]
So, Wendy, as you mentioned earlier: bird flu can be fatal, which is the most worrisome aspect, particularly for threatened or endangered birds. So what are the potential interventions to this threat and is vaccination on that list?
Wendy Puryear: Within the US, it was the case with the condors that there were a pretty high number that were getting infected and were dying from the virus, and when you're talking about a species that's critically endangered and you lose 10 or 20 percent to a virus, that's a really bad situation.
So there was a vaccine that was rolled out in that scenario. It's something that would be considered for other populations, for example, gray seals and harbor seals, those populations are doing pretty fine, they're large populations. That's not something where people are talking about vaccinating.
If it were to start to show up in a Hawaiian monk seal that's critically endangered, that's a situation where a vaccine would make sense to move forward.
There are some countries that are actually already vaccinating poultry and that is something that's being discussed. It's not something that is approved within the U.S. yet for an influenza vaccine, so within a poultry setting that is an option. It's impacting so many different species that vaccinating all animals on the entire globe is clearly not possible. But there are cases where it might make sense.
And then for human health, because the virus is a different form of what we already have for seasonal influenza, the vaccine that we currently get isn't perfectly matched for this bird flu form. So we would need to tweak it and adjust it. But that groundwork has already been done. So there's already a stockpile of like, a seed stock, to be able to fairly rapidly grow up and roll out. If it looked like it was necessary to do that for a human health point of view, that there would be that vaccine.
Deja Perkins: It's great to know that they're already on top of that.
Wendy Puryear: Right.
Deja Perkins: Can you share with us, from a virologist's standpoint, how bad is this, and how worried should your average bird lover or poultry lover be?
Wendy Puryear: From my perspective, watching this unfold over the last couple of years, it's been the scenario where it'll be like, ‘Well, it's made it into migratory birds and that's really unsettling but at least it hasn't gone into species X.’ And then that happens.
[Then it’s] like, ‘Oh, all right. Well, at least it hasn't gone into mammals. Oh, okay. It went into a fox. Well, at least it's only gone into a couple of fox. Oh, well, it's gone into a caustic outbreak in seals. Well, at least it was—’ Like, it keeps going a step further and further and further. So it keeps becoming more and more concerning.
And I feel like it's one of those things that, that we're, we're kind of slowly watching the dominoes fall. It's been from the virology point of view, very unsettling to watch it kind of build momentum and going into now one of the primary agricultural food sources for humans, into domestic animals where it's showing up in more and more cats that are impacted and still a low level of human infections, so that is reassuring. But it keeps kind of dripping at the human infection.
With all that said, at least from the human health point of view, I do find reassurance in the fact that this is not COVID.
[Music starts]
So, COVID was a situation where it was a virus that was not on our radar. It suddenly came from out of nowhere. We had to figure out what it was and then we had to figure out how to respond to it, and we had to roll out a response. So we had to very rapidly get up to speed on something that we were starting from zero.
We know what this is. We see it coming. We have a lot of experience with influenza. The problem is that because it's an RNA virus and because things can change so quickly and because there's only so much public will - and we all have pandemic fatigue - there's a fine line to cross between: you don't want to roll out a vaccine too early and to have it not be quite perfectly matched with whatever the most problematic version is going to be. And you don't want to roll it out too late and then miss that window to try to intervene as effectively as possible.
So there's a really careful balancing act that's being done. I am more concerned for the wildlife side of things. Other than stepping in if it's a critically endangered species and it's a, a smaller population that we can try to vaccinate and have some sort of impact on. But, to a large extent, there's not a whole lot that we can do in that setting and that's the most concerning part for me.
Deja Perkins: Yes, that is very concerning.
You mentioned that this isn't the same situation as COVID in 2020, as far as unpreparedness, which is great. But do you see any parallels between this outbreak and the COVID 19 pandemic?
Wendy Puryear: They are very similar viruses in some regards. So they're both RNA viruses.
You can be RNA based or DNA based. So, we are DNA based. DNA is much more stable. The reason it's important that it's an RNA virus is RNA is inherently sloppier in how it replicates.
So, every time it makes new copies of itself, it is introducing sub mutations each time. So that means that RNA viruses are much more capable of changing very rapidly and being able to potentially move into other species more rapidly because they're going through all of these changes that might allow them to sort of, just by happenstance, stumble across the best way to infect another species.
So that was true for both SARS CoV 2, the virus that caused COVID, and for influenza and high path influenza as well. They're both respiratory viruses. The things that protected us from COVID infection, also protect us from influenza infection.
So we have learned the public health measures that could and should be implemented if there were to be a human health concern for this virus. You know, masks would certainly help with influenza and hand washing and all the lessons that we learned through the COVID pandemic still apply to influenza. But then, also, the wild animal connection. And the agricultural and the food source connection, because there are a lot of similarities with how COVID made its way into the human population and where high path form of influenza develops in these densely populated poultry settings.
So there are ways that we globally think about how we could adjust our agricultural practices and, and the way that we could potentially adjust some of the ways that we manage our food sources to hopefully not have these sorts of things keep cropping up again and again and again.
[Music transition]
Deja Perkins: Purbita, Back to you.
Purbita Saha: Thanks, Deja.
[Music stops]
Speaking of COVID, many of us might remember that the government response to the pandemic was highly scrutinized, and really, still is. And, so far, the bird flu outbreak is a similar story.
Since early June 2024, many scientists, including virologists, have gone on record to discuss what they perceive to be the U.S. Government’s lackluster response to bird flu, specifically after the very first outbreak in dairy cattle this spring.
Their concerns include a lack of data and slow responses from leading organizations like the CDC and USDA; slow dissemination of information; and a higher risk of the virus mutating given mammal to mammal transmission. Critics worry that these things could squander our chance to prevent another pandemic.
But Wendy has a different view on the backlash.
Wendy Puryear: Of course, everybody always wants more and faster, right? Myself included. But I know a lot of people who work at the USDA and USGS and CDC and the state agencies and state vets.
And I can attest to the fact that everybody is working their tail off. So the fact of the matter is, this is an outbreak that has been going on already for two years. And everyone is in overdrive all the time and it just doesn't let up. And then it keeps shifting into new things and there are only so many resources available.
So, yes, there are frustrations. I wish it was faster and that all of that was happening in a more streamlined manner but given the reality of the humans trying to make it happen on the resources that are available, I'm actually pretty impressed with how well it has worked. And that people have been so proactive in trying to reach across all these different agencies and to work together and to try to share info as quickly as possible.
Andy Ramey: I want to clarify that the USGS is tracking avian influenza, not just through anecdotal methods, but really through carefully planned, scientific testing of samples.
And the USGS is just one agency.The USDA also conducts surveillance, both active surveillance, like I just described, and also through passive surveillance, that is the reporting of sick and dead birds.
So, the USGS and USDA certainly do not work in isolation. We work with a variety of academic partners, state agencies, in order to get data that really helps us to better understand what's going on across the landscape throughout the United States.
And I think similar programs are in place, for instance, in Canada.
Purbita Saha: While scientists are busy monitoring the progress of bird flu, Wendy says that for people who are more prone to exposure — whether on a farm or at work — there are a few things that can be done to limit the spread of the disease.
Wendy Puryear: There's a lot of high path influenza that is out there and that is circulating.
So if you have an open backyard bird setting where other birds, for example, crows and ravens, might come around frequently. So if those animals are shedding virus through their feces into the area where you have your backyard chickens, that is absolutely a transmission opportunity that can happen, and chicken, they are incredibly susceptible to this virus.
So really trying to limit those interactions would probably be the first most important piece of information to relay. The second most important information is that interface between domestic animals and wild birds. So, if you have a domestic cat and they are then potentially interacting with birds, that is absolutely a place where those cats can end up becoming infected with high path influenza. And we for sure know that cats are susceptible.
If you are somebody who is walking your dog out along the beach or through a wooded area and you come across a bird carcass, and your dog, like most dogs, gets super excited about rolling around on the body of that bird carcass that it comes across, biting hold of it, or it sees a sick injured bird that becomes an easy target for it to play and grab hold of with its mouth– absolutely a possibility that that dog is going to get infected. So those are the places of the highest concern.
We haven't seen it a whole lot in songbirds. That is starting to shift a little and I would couch that with if any of your listeners are within an area where there have been the dairy outbreaks, there are starting to be more and more reports of peri domestics, of sparrows and finches that have high path influenza in close proximity to those farms. So there is the possibility that it can get into songbirds. So it's not a widespread situation yet, but that would be something to watch about.
Purbita Saha: That’s helpful to know. So, Andy, is there anything about this virus that could make it less of a threat overtime?
Andy Ramey: I'm personally not very optimistic that this problem is going to resolve on its own anytime soon. That stated, I think there's ways we might be able to live with this disease burden better.
I think if wild birds are provided good quality habitat in which their populations can thrive and individuals can live their healthiest life, these populations are likely to show resiliency. I think there'll be many healthy birds that will be able to maintain healthy populations, in light of the fact that highly pathogenic avian influenza might be out there on the landscape at some level.
More recently, there have been less confirmed detections among wild birds. That could be, in part, to more attention being given to domestic animal outbreaks, which are obviously a major concern. This could also have to do with increasing population immunity among wild birds in North America.
So population immunity refers to the presence of antibodies or natural protection of populations. So as more birds became infected with highly pathogenic avian influenza, those that survived may have developed antibodies protecting them from future infection. And this Increased population immunity might slow down transmission of highly pathogenic avian influenza among wild birds in North America.
So I should clarify that there's many types of low pathogenic avian influenza that are circulating among wild birds, and those birds that are exposed to low pathogenic viruses might be less likely to develop disease or to die on account of highly pathogenic avian influenza.
Purbita Saha: And for people who may be less prone to exposure, there are things you can also do to help, from environmental advocacy to biosecurity awareness.
Wendy Puryear: From the perspective of habitat loss, more wildlife are trying to all coexist on less real estate and interacting with each other more because there's just physically not as much space for them to spread out. You know, if there's less and less beach available, the birds are coming down in a higher density to the same place where the seals are coming down, that helps to feed that sort of thing.
When we densely populate food species in together, that creates an environment where these viruses are able to evolve and take hold and spill into human populations, and with the case of high paths, spill back out into wildlife.
More immediately doable is our biosecurity practices. So if you're talking about backyard poultry or if you're talking about commercial poultry, really on top of the biosecurity that's in place in the case of a farm, if you're moving from one farm to the next, if a delivery truck goes from one farm to the next farm, that could be bringing virus along with it.
On a more personal level, if you are out birdwatching and you're in one area, and especially if you see any signs that there could be neurologic birds or you see dead birds, it would be prudent to not then go four miles down the road to another marsh and go birdwatching down there because there is the possibility that you've now picked it up on your shoes and you're going to transit it down and potentially help to escalate that virus down further.
Purbita Saha: Another important factor is food consumption. Since bird flu is affecting farmed animals, everyone should stay in the know about both local and global guidelines for food safety. And Wendy says awareness about milk, in particular, is vital.
Wendy Puryear: The current outbreak situation as it's gone into dairy cattle is that infected cows shed virus that is still infectious at really high concentrations in the milk. Pasteurization kills it and is very effective. So pasteurized milk, there's no reason to think that that is a concern. Raw milk is a concern. So there have also been a lot of reports of the sale and consumption of raw milk actually increasing since High Path has been reported in dairy cows.
And that is definitely creating a situation where there is an opportunity for things to go really bad. So I would love to see that practice change. But the pasteurized milk, by all measures, is completely killing anything that's coming through there. The raw milk is not.
Purbita Saha: The USDA released food safety guidelines to help ensure that the consumption of meat, eggs and poultry is safe, as long as they are properly prepared and cooked.
The USDA suggests cooking beef medium to well done - or 145° to 160°F - “to kill the H5N1 virus”. If you prefer to eat beef rare, cooking it to 120° should “inactivate the virus”. For ground meat and poultry, they recommend cooking it to at least 165°, standard with all poultry food safety recommendations.
We encourage everyone to read the USDA guidelines for food handling and kitchen safety. There’s a link to those guidelines on the BirdNote website.
Purbita Saha: And finally, where do you rate this strain of avian flu? How worried should we be? And do you have any words of encouragement?
Andy Ramey: Highly pathogenic avian influenza certainly seems like a significant stressor on wild bird populations to date. That is, when we think about the number of birds that have been affected, the breadth of species that have been affected, and the fact that there's no sign that this virus is going to be extirpated anytime soon, I think it has to be up there among the contenders of causing greatest impacts on wild birds across the landscape.
That being stated, I think wild birds are resilient and I think, with conservation measures to provide good habitat and to support healthy bird populations, I'm hopeful that this is a stressor that birds will be able to show resiliency towards. Though, I think we shouldn't take that for granted.
Efforts that people are making to help support conservation of wild birds and wild bird habitats, are ultimately going to be useful for promoting avian health. And so, I applaud those efforts and I think they're helpful and I'm hopeful it will encourage healthy populations of wild birds across North America moving forward.
Purbita Saha: All right. Thank you, Andy…
Deja Perkins: And Wendy, thank you so much for joining us on the show today…
Purbita Saha: It's been a great opportunity to learn from one of the leading experts on this virus.
Deja Perkins: And educating us about the current status of the bird flu.
Andy Ramey: I really appreciate the invitation to speak with you today.
Wendy Puryear: Absolutely. It was a lot of fun to be here and to talk with you
--
Purbita Saha: Birds are all around us, which means the viruses they carry are, too. That might sound scary—but the point is, each of us can play a big role in tracking the course of this outbreak and keeping our fellow beings safe.
Birders, livestock owners, hikers, hunters, and wildlife rehabbers should stay alert for injured or dead birds, especially during migration season. Infected animals can show a wide range of symptoms like coughing, swelling, and trouble breathing, walking, or flying. If you think you’ve come across bird flu at a public park or green space, report it to whoever manages the property so they can scope it out safely. If the animal is on your land, contact your state veterinarian.
In either case, keep your distance from the body and let the experts decide what to do next. As we know all too well, this virus doesn’t stick to birds, despite its name.
And in case you missed our last episode, here’s some good news: You don’t have to take your bird feeders down. Just clean them out like you normally would to keep a sanitary environment for your hungry visitors.
It’s been a tough few years with pandemics and epidemics and all these reminders of how fragile life is. But, you know what? Birds are tough, too. They survive harsh elements and marathon migrations. They survive glass fortresses, toxic spills, and noise pollution. And they survive and adapt alongside the viruses that are undeniably part of the world—and they can teach us to do the same. Maybe that is the light at the end of the tunnel.
[Music break]
Purbita Saha: Many thanks to Andy Ramey and Wendy Puryear for their thoughtful answers and impactful work during this critical time.
Deja Perkins: And That’s a wrap for season 6! We covered quite a lot from community building and bird collision advocacy in Chicago to the importance of female birds and ornithological research in the Neotropics. We’d love to hear your thoughts and feedback about your favorite episodes and moments. And we hope you’ll continue to share these episodes with your family and friends.
It was a pleasure co-hosting with you, Purbita!
Purbita Saha: Same here, Deja!
For more about bird flu, our guests, ways to protect yourself and the animals around you, plus other resources from this episode— please visit BirdNote dot org.
And don’t forget to follow us on Instagram, @ Bring Birds Back, for the latest updates about the show.
Bring Birds Back is created by our production team, including producers Mark Bramhill and Sam Johnson; Managing Editor, Jazzi Johnson; Fact-checker, Ariana Remmel; and our Content Director, Jonese Franklin.
Our music is by Cosmo Sheldrake and Blue Dot Sessions. And this episode was hosted and co-produced by me, Purbita Saha.
Happy birding everybody! Until next time…
Dr. Andy Ramey currently serves as the Director of the Molecular Ecology Laboratory for the USGS Alaska Science Center located in Anchorage, Alaska. He oversees a research program focused on wildlife health and disease, populations genetics, and environmental DNA. Andy has undergraduate degrees in Fisheries and Wildlife Biology from Colorado State University and a Ph.D. in Veterinary and Biomedical Science from the University of Georgia. Andy has spent his entire professional career working for the Department of Interior in Alaska, including more than 20 years of experience working at the USGS Alaska Science Center. Outside of work, he enjoys hiking, paddleboarding, skiing, wildlife photography, and flyfishing.
Dr. Wendy Puryear is a Scientist at the Cummings School of Veterinary Medicine at Tufts
University, studying how viruses are maintained, spread, and evolve in wild animals. She was
trained as a molecular virologist at the University of Washington, where she completed her PhD
in 2006. She is especially interested in understanding the wide range of factors that impact
infectious disease, from adaptations of the virus itself, to the impacts of environmental
contaminants, shifting populations, and climate change. In the thick of winter, she spends much
of her time organizing and conducting field work on seals off of Cape Cod, where the largest US
pupping colonies of grey seals are located. Throughout the year, she works closely with wildlife
professionals and stranding networks to look at wildlife ranging from birds to terrestrial and
marine mammals. Back at the lab, she works to determine which viruses are circulating in wild
animals and tries to unravel how and why certain viruses persist. Her current research focus is
on Influenza, including High Path Avian Influenza, morbillivirus, and SARS-CoV-2.











